Take Care of Your Mental Health This Holiday Season
The holiday season brings different emotions that are often joyous, but for some, it can be a somber time of year. It’s important to consider the impact the holidays may have on your mental health.
Many are still finding difficulties navigating the ups and downs of the season, all the while, they are planning, attending and engaging in activities such as work parties and family gatherings. This may be due to the loss of a loved one, inability to gather as a family, or financial difficulties among other things. However, taking time to focus on the things you can do may help shift your focus.
First Things First – This Is Hard
As we turn the calendar to another December, remember we have been living through a pandemic that caused changes to routines, physical distancing, isolation, loss, and uncertainties for a few years now. With the holiday season here, it may be the first major event with family in a few years, or it could be the first time without a loved one. Try to remember we are all experiencing emotions through this – some similar and some different – but you aren’t alone and that can help you cope.
The Highs and Lows of Holidays
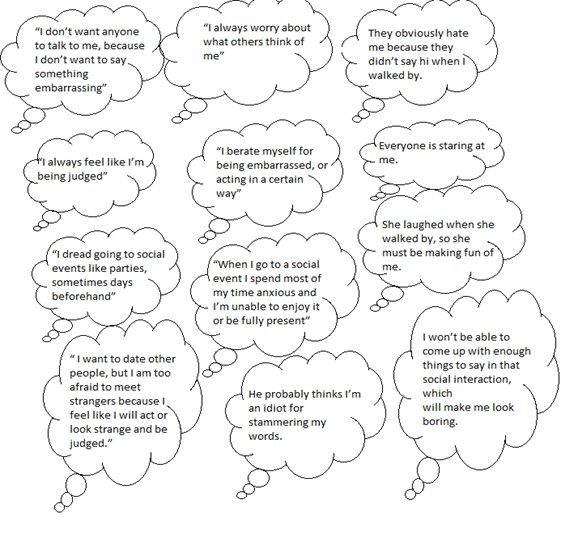
People face a lot of emotions during the holidays. This can be from not having family, having lost loved ones, living far away, or feeling overwhelmed by all the expectations and demands of the season. We should expect these feelings in ourselves and others.
Don’t avoid these feelings, recognize them. We can also expect these feelings to come in waves. The first wave will probably be the biggest, emotionally, and then it can become more manageable from there.
The important thing is to know yourself and expect some ups and downs. But the second most important thing to remember is that it’s best to embrace the feelings and work through them rather than trying to stop these feelings altogether.
Take Action
Knowing yourself is key to the entire process of mental and emotional health during the holidays and throughout the year. Try to understand your triggers – something that can make you feel sad, angry, overwhelmed – and be prepared.
The next step is to have coping skills, or actions you take to deal with the highs and lows. These skills will be a big part of working through things as they happen, even more so to help with holidays and mental health. Some coping skills can include:
- Talking to someone
- Making a list
- Doing deep breathing exercises
- Going for a walk
- Or writing in a journal
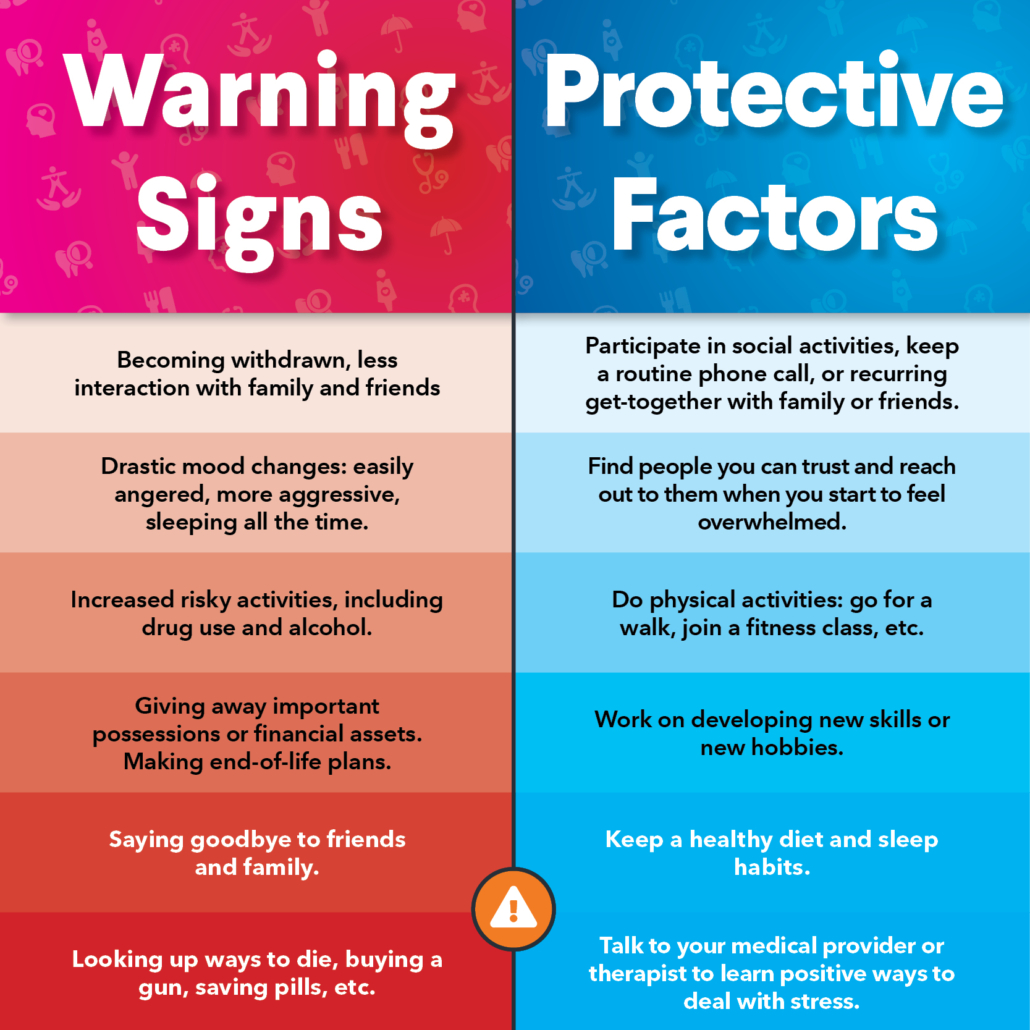
Another way to be proactive is to notice changes in other people and yourself. Some of the most common changes can be withdrawing from activities, isolating, not contacting people, sadness, and not enjoying hobbies. These can be red flags during the holidays and may spark mental health concerns.
It’s OK to Feel Lonely
It can be very uncomfortable to feel lonely, but it is okay to feel lonely. It is a very normal emotion, even more so when we have expectations of something different.
Dealing with this can happen in a few ways.
- Throw out the idea of “should”. For example, don’t continually think or say “I should be able to be with my family” or “I should be going on a trip”. It’s fine, and even good, to mourn a lost holiday or celebration with people you care about, but then take those options out. Think about what you can do and focus on that this year.
- Change your expectations. This is a good rule any time of year. We set high expectations of ourselves and of the holidays, which can lead to disappointment. Rethink or lower your expectations to something more realistic.
- Use this opportunity to help others who may also be facing loneliness like a neighbor, an elderly friend or family member who has been isolated, or one of your kid’s friends who has family that is working during the holidays. Find ways to show people you care, that they aren’t alone, and make new memories. You will be surprised how much good it does for that person, and for you!
Loneliness is a big factor on holidays and mental health of people everywhere. Efforts in this area can make a big difference.
Know When to Ask for Help
We believe in prevention in healthcare, whether it is physical health or mental health. If you have been struggling, make an appointment with one of NOAH’s counselors or psychiatrists now.
People who are at a higher risk, or who deal with chronic depression or anxiety, should be seeing someone on a somewhat regular basis, especially if holiday stress or loneliness would trigger more emotions. Another warning sign is isolation. If you notice yourself isolating more or see changes in a loved one with their moods or interactions, that is a good time to make or encourage an appointment. Everyone can benefit from counseling.
Find Ways to Enjoy the Season
Now that we are ready to adjust our expectations, embrace the emotions of the season, and know what to expect, we can find new ways to celebrate the season safely for our mental health.
Make your plans – If you want to do a video call with multiple family members, make those arrangements. Remember that some people may not have reliable WiFi or be comfortable using certain technologies so plan accordingly. Making phone calls to loved ones and sending cards are ways to share the season with people you care about.
Remember to also be thankful and show gratitude which is helpful to your mental and emotional health all year. Showing gratitude to your family, friends, coworkers, neighbors and even strangers can have a ripple effect. So, hold the door open, smile, give a compliment, or make small talk with the cashier, and you will brighten many people’s day in the process.
If you need a counselor, reach out to NOAH’s team of experts. Virtual visits are common and can fit in your schedule and lifestyle.