May is Mental Health Month
We live in a rapidly changing world that can be complex to navigate. Nearly half of Americans are able to remember a time were there wasn’t a need to constantly connect and it was easier to tune out the noise of the world, while the younger half of the population can’t imagine life without the internet.
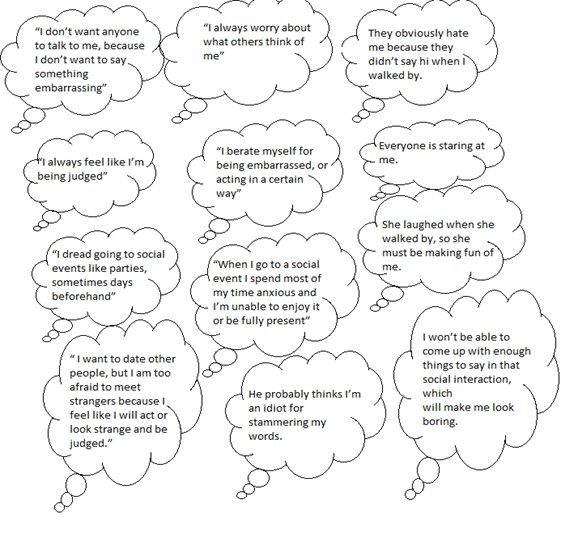
Modern life can have a significant impact on mental health — for better or for worse. The disturbing imagery in the media we are exposed to today can be deeply unsettling. At the same time, our current technology also allows us to mobilize and provide collective support more efficiently in times of natural disasters or injustice.
And ironically, while our devices make us more connected than ever, loneliness is an increasingly serious public health concern. We are now able to have conversations with friends and family on the other side of the world in real time. However, constant connection also means that we will know if we weren’t invited to a friend’s party down the street. Recent survey data show that more than half of U.S. adults (58%) are lonely.
Finding a sense of calm and focusing on well-being when you are having mental health concerns can be daunting in our fast-paced society. It can be especially challenging to know where to start.
May is Mental Health Month and NOAH is raising awareness of the important role mental health plays in our lives. We are encouraging members of the community to take action toward protecting their mental health and overall well-being.
This May, NOAH will focus their efforts on helping members of the community to:
• LEARN how modern life affects mental health with new resources to navigate our changing world.
• ACT by building a strong mental health program through our integrated model of care.
• CHAMPION to improve mental health for our patients and community.
If you think you may be experiencing symptoms of a mental health condition and are unsure of where to start, give us a call at 480-882-4545 and schedule an appointment with your NOAH provider. It’s important to remember that working on your mental health takes time. Change won’t happen overnight. Instead, by focusing on small changes, you can move through the stressors of modern life and develop long-term strategies to support yourself — and others — on an ongoing basis.
Read more