Dental Tips for National Children’s Dental Health Month
By Nicollette Villescaz, Pediatric Dental Assistant
Even as the shortest month, February brings a lot of holidays and awareness topics. One awareness topic not to be missed is National Children’s Dental Health Month! My name is Nicollette and I am a professional pediatric dental assistant here at NOAH. I’m going to share pediatric dental tips on how parents and caregivers, along with your child’s dental team can work together to prevent tooth decay, which is the number one dental problem for preschoolers with around 50% of children having one or more cavities by age 5.
Dental tips to prevent tooth decay in your child
The best way to ensure healthy teeth is to prevent problems before they start. Things like having a healthy diet, proper brushing and flossing habits, and not having sugary drinks from baby bottles can help protect your child’s teeth.
Rethink your drinks
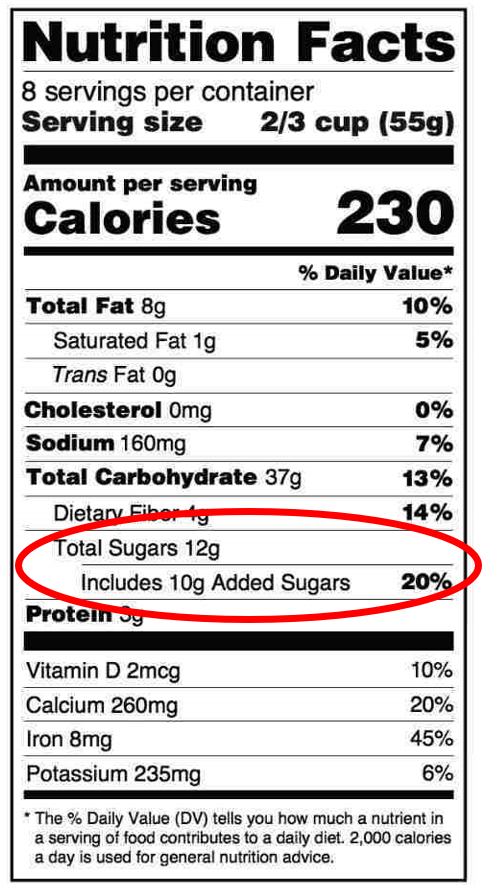
As parents and guardians of young children, we know that a healthy diet is important, and we shouldn’t give them candy and sweets too often. However, it’s actually what children drink, not what they eat that is more dangerous to their teeth. I have heard and seen our NOAH dentists and medical doctors express repeatedly how bad juice, soda, energy drinks, Gatorade, and lemonade are for children. They aren’t bad for kids just because of the artificial flavors, and dye colorings, but also because of the high amounts of acid and sugar. These drinks have too much sugar and acid for kids of any age. The only fluids a child needs are plenty of water (especially in this desert heat) and milk for nutrients like calcium. When parents and caregivers give children acid and sugars to eat and drink we are putting them at a greater risk for tooth pain caused by cavities.
Brush and floss
Children and parents need to know the right way to brush and floss those little teeth because baby teeth are so important to keep healthy. Our top priority when children and parents or caregivers come to NOAH Dental is education and prevention. There are stages to this as kids grow:
- As soon as teeth appear, it’s time to brush! A few tiny baby teeth need just a small amount of cleaning.
- When more teeth arrive, increase brushing. Parents and guardians need to help children brush their teeth twice a day. Kids can’t brush all the cavity-causing germs and crumbs away by themselves.
- Once a child is old enough to brush their own hair or tie their own shoes, then they can start to brush and floss on their own.
- Stay consistent at every stage. A dental hygiene routine is vital to healthy teeth.
Ditch the bottle
The biggest contributor to cavities in our infant and toddler patients is the bottle! Babies should never have anything other than water or milk. Once a child is a year old, they should only have milk with meals, not nap times or throughout the day – stick to water for that! Letting kids drink milk or juice any time of the day, puts them at risk for tooth pain caused by cavities.
Care for those baby teeth
Too often I hear parents or guardians say, “They are just baby teeth, it’s not so serious,” and “They will be falling out anyway.” This is where our dental education is so important! Children experience the same effects of a toothache exactly how an adult would, with cold sensitivity, difficulty drinking or eating, throbbing pain, swelling, infections, and difficulty sleeping. Children need healthy teeth to help them chew and speak clearly. Plus, baby teeth hold the space for their adult teeth to come in correctly.
Cavities and dental pain are preventable in children. The NOAH Dental team works together with parents and guardians to keep away tooth decay and pain away in children. To learn more, visit our NOAH Dental page for helpful videos and tips. If you are ready for you or your child to see a NOAH dentist, make an appointment today!