Take Care of Your Mental Health This Holiday Season
The holidays can bring joy, but it can also be a difficult time for many. It’s important to consider the impact the holidays may have on your mental health.
Many people find difficulties navigating the ups and downs of the season. This may be due to the loss of a loved one, inability to gather as a family, or financial difficulties among other things. All the while, they are planning, attending, and engaging in activities such as work parties and family gatherings. However, taking time to focus on the things you can do may help shift your focus.
Acknowledge Your Feelings
People face a lot of emotions during the holidays. This can be from not having family, having lost loved ones, living far away, or feeling overwhelmed by all the expectations and demands of the season. We should expect these feelings in ourselves and others.
Don’t avoid these feelings, recognize them. We can also expect these feelings to come in waves. The first wave will probably be the biggest, emotionally, and then it can become more manageable from there.
The important thing is to know yourself and expect some ups and downs. But the second most important thing to remember is that it’s best to embrace the feelings and work through them rather than trying to stop these feelings altogether.
Take Action
Knowing yourself is key to the entire process of mental and emotional health during the holidays and throughout the year. Try to understand your triggers – something that can make you feel sad, angry, overwhelmed – and be prepared.
The next step is to have coping skills, or actions you take to deal with the highs and lows. These skills will be a big part of working through things as they happen, even more so to help with holidays and mental health. Some coping skills can include:
- Talking to someone
- Making a list
- Doing deep breathing exercises
- Going for a walk
- Or writing in a journal
Adjust your expectations for the season to fit your current reality. By letting go of perfection and embracing what’s possible, you may find new ways to experience the holidays.
It’s Okay to Feel Lonely
Loneliness is common during the holidays, but it doesn’t have to define your experience.
Dealing with this can happen in a few ways.
- Throw out the idea of “should”: For example, don’t continually think or say “I should be able to be with my family” or “I should be going on a trip”. It’s fine, and even good, to mourn a lost holiday or celebration with people you care about, but then take those options out. Think about what you can do and focus on that this year.
- Change your expectations: This is a good rule any time of year. We set high expectations of ourselves and of the holidays, which can lead to disappointment. Re-think or lower your expectations to something more realistic.
- Use this opportunity to help others who may also be facing loneliness: Reaching out to someone else—whether it’s a neighbor, an isolated relative, or a friend—can create meaningful connections and help both of you feel supported. Small acts of kindness can have a big impact, especially during this season.
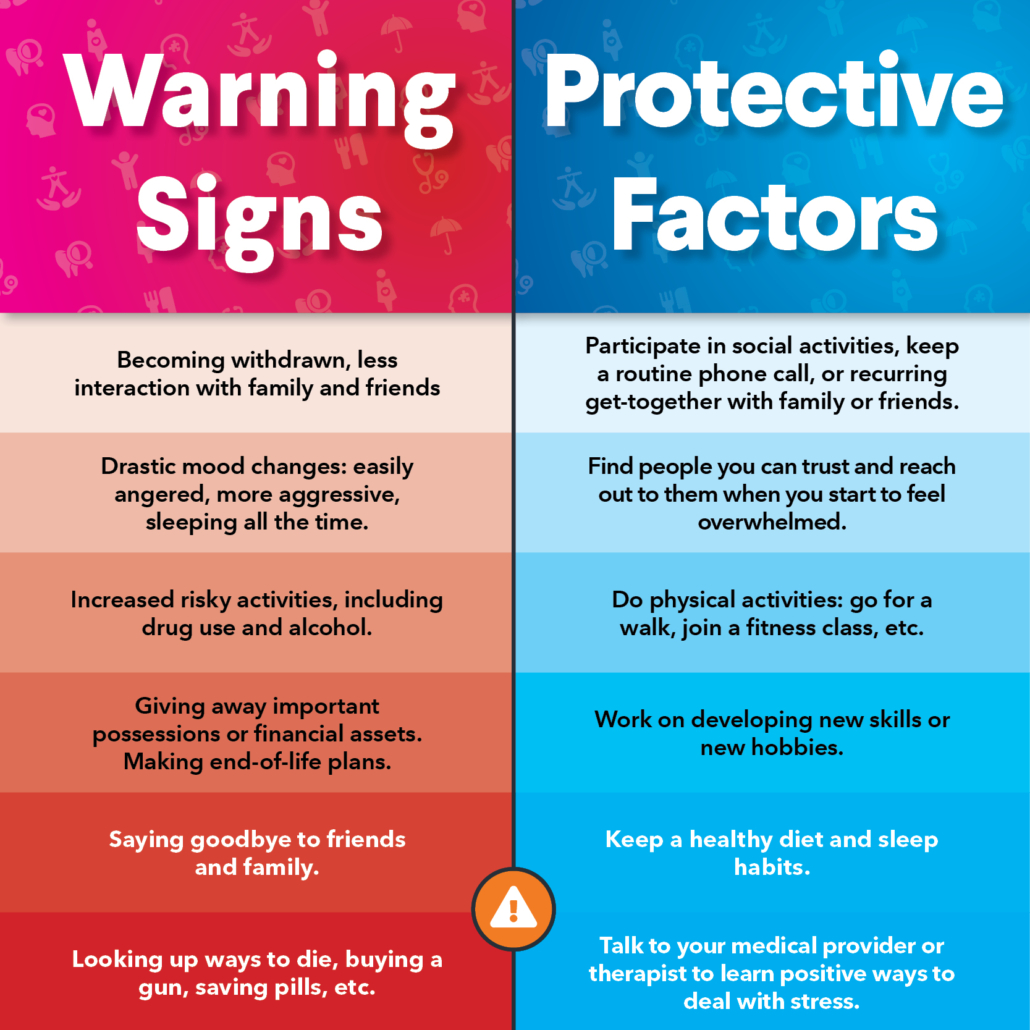
Know When to Ask for Help
We believe in prevention in healthcare, whether it is physical health or mental health. If holiday stress becomes overwhelming, or if you notice changes in mood, behavior, or interest in yourself or a loved one, it may be time to seek professional support. NOAH’s counselors and psychiatrists are here to help you navigate these challenges and improve your mental well-being.
Find Ways to Enjoy the Season
Now that we are ready to adjust our expectations, embrace the emotions of the season, and know what to expect, we can find new ways to celebrate the season safely for our mental health.
Make your plans – If you want to do a video call with multiple family members, make those arrangements. Remember that some people may not have reliable WiFi or be comfortable using certain technologies so plan accordingly. Making phone calls to loved ones and sending cards are ways to share the season with people you care about.
Remember to also be thankful and show gratitude, which is helpful to your mental and emotional health all year. Showing gratitude to your family, friends, coworkers, neighbors, and even strangers can have a ripple effect. So, hold the door open, smile, give a compliment, or make small talk with the cashier, and you will brighten many people’s day in the process.
For additional help, request an appointment here. Our expert providers are ready to offer you the support and care you may need during this holiday season.