Everything about COVID-19 came at us quickly in 2020. From how the virus spreads to vaccine options, we have learned so much about. But it’s also no surprise that there are questions and misunderstandings. That’s why NOAH experts are responding to some of the most common COVID vaccine myths.
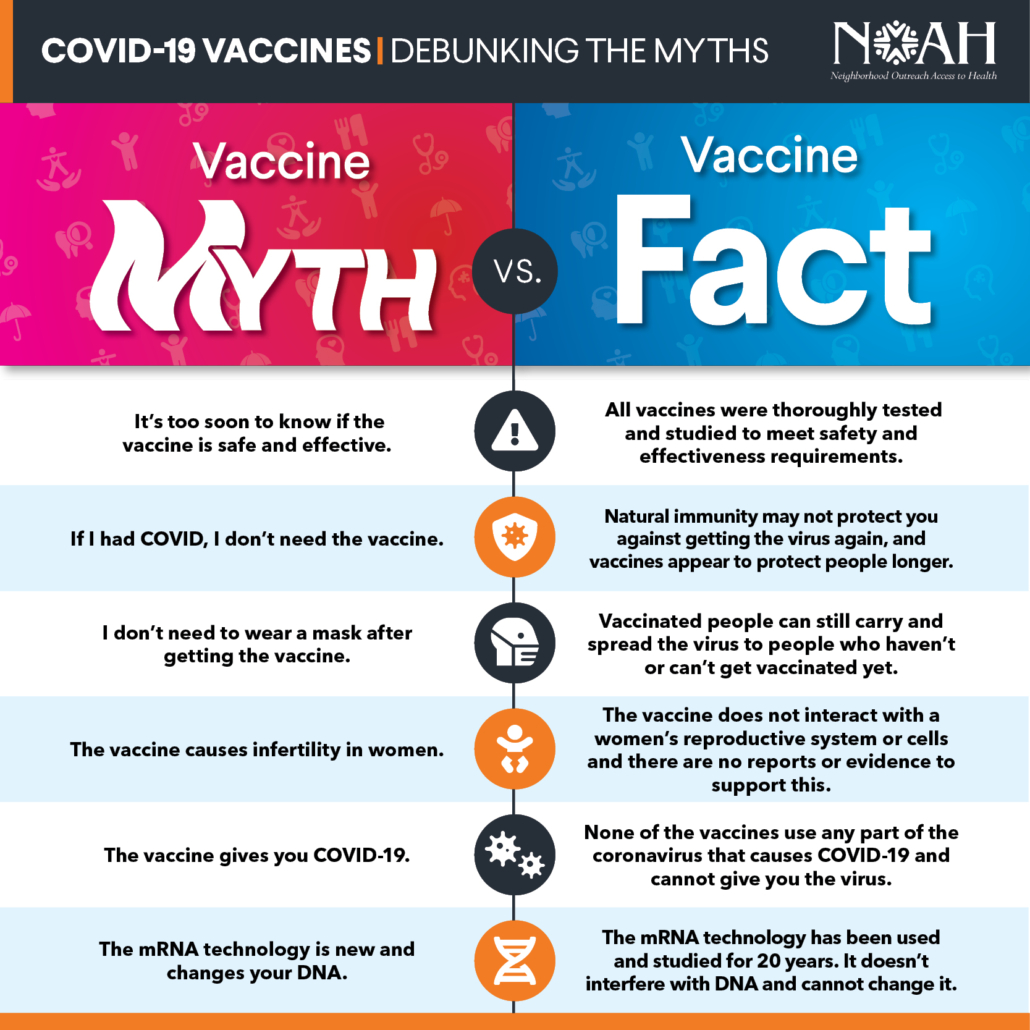
Myth #1 – It’s too soon to know if the vaccine is safe and effective.
Fact – Approved vaccines – Pfizer, Moderna, and Johnson and Johnson – did not skip any necessary step. The two initial vaccines approved in the U.S., Pfizer and Moderna, were about 95% effective in trials. The Johnson and Johnson vaccine is 66.3% effective in preventing all COVID-19. All available vaccines are highly effective at preventing infection, as well as preventing hospitalization and death from the virus.
The vaccines are safe. Other than expected side effects like headaches, chills, and arm pain, severe allergic reactions are extremely rare. All patients are monitored for 15 minutes after receiving their vaccine to monitor for any signs of these rare reactions so they can receive immediate treatment if needed.
Myth #2 – If I had COVID, I don’t need the vaccine.
Fact – People can – and have – gotten COVID-19 more than once. Plus, this virus can have serious and lasting health risks. We also don’t yet know how long natural immunity (from having COVID-19) will last. Early evidence shows that natural immunity may not last long enough to stop the spread. The evidence scientists are seeing from the vaccine tell us that the vaccine may offer better protection than natural immunity.
Myth #3 – I don’t need to wear a mask after getting the COVID vaccine.
Fact – Fully vaccinated people can still carry and spread the virus to unvaccinated people. By wearing masks and continuing to give physical distance from people that don’t live in your home, you are protecting them from infection, and from you getting the virus and carrying it to other unvaccinated people.
At this time (4/5/2021), none of the vaccines are approved for children under 16. Those trials are underway but are not fully approved yet. Wearing your mask will continue to protect children and other unvaccinated individuals.
Myth #4 – The vaccine causes infertility in women.
Fact – None of the available COVID-19 vaccines cause infertility. This myth happened because a false social media report (*read more on this at the end) was shared saying that the spike protein on the coronavirus was the same as another spike protein that is involved in placenta growth and attachment during pregnancy.
The spike protein in the coronavirus is what allows it to enter the cell and replicate. The vaccine targets this spike protein.
The false report said the COVID vaccine would target the protein in a woman’s body that helps with healthy placenta growth and harm her fertility. The COVID vaccine ONLY targets the specific spike protein of the coronavirus because it is completely different. The vaccine won’t interact with a woman’s fertility or fertility treatments. More information from Johns Hopkins Medicine on this topic is available here.
Myth #5 – The COVID vaccine gives you COVID.
Fact – The COVID vaccines by Pfizer and Moderna use mRNA technology and do not use any form of any virus. The Johnson and Johnson vaccine uses what is called a viral vector to carry the information to our body. This vector is a harmless version of a different virus. None of the vaccines can give someone the virus because none of the vaccines contain any part of the virus. What all of the vaccines will do, though, is tell our healthy cells how to respond to COVID-19.
Any side effects from getting the vaccine, like arm pain where you received the shot, a fever, body aches, chills, or a headache are actually a good thing! We know they aren’t fun, but they are temporary and show that your body is responding to the vaccine and building protection. Many people don’t experience any side effects.
Myth #6 – The mRNA technology is new and changes your DNA.
Fact — The Pfizer and Moderna vaccines use mRNA technology to give instructions to our bodies on how to fight the virus that causes COVID-19. The mRNA does enter the cell, but does NOT enter the part of the cell that contains our DNA, so it cannot change our DNA.
This mRNA technology is not new to science or medicine; it has been used and studied for almost 20 years. The COVID-19 vaccine is the first time, though, mRNA is being used in a vaccine. Scientists were able to create the vaccines happened faster than if scientists were using a new technology because of past experience and studies.
NOAH’s own Dr. Bell shares a helpful and easy-to-understand information about COVID-19 and the vaccine in this brief YouTube video.
So much has happened around COVID-19 in just one year. Ensuring our patients and community understand how to stay safe and healthy is important. Your NOAH provider can answer any questions you have about COVID, the vaccine, or any other health and wellness concerns. Check out the NOAH COVID-19 page on our website for additional information.
*Social media allows us to stay connected and to share helpful, fun, and important information with people in our lives. However, the prevalence of misinformation shared across social media platforms can cause real and harmful outcomes. At NOAH, we only share our NOAH provider’s (doctors, physician assistants, nutritionists, counselors, nurse practitioners, psychiatrists, dentists, etc.) expert insight and knowledge, or trusted third-party sources of information. We will never share questionable information, rumors, or unverified medical insights in our blogs or on our social media platforms.